A spinal cord injury (SCI) is damage to your spinal cord that can disturb the flow of nerve signals between your brain and the rest of your body. This can lead to loss of movement, sensation or function below the injury site.
The extent of your SCI, and the symptoms you experience, relate to the spinal vertebrae (bones) where the injury occurred. There are 7 cervical vertebrae (C1 to C7) at the top of your spine, 12 thoracic vertebrae (T1 to T12) in the middle of your spine, and 5 lumbar vertebrae (L1 to L5) which attach to the sacral bone (the sacrum) and pelvis at the bottom of the spine.
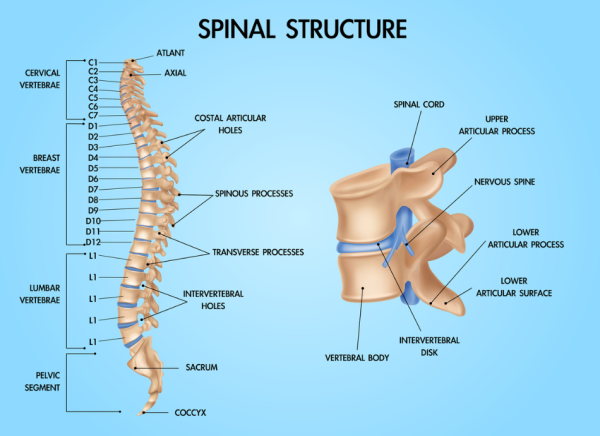
Image credit: Depositphotos
SCIs can be caused by trauma, such as accidents or falls, or by diseases such as multiple sclerosis, spine infection, spinal canal stenosis or spinal tumours. The effects can vary widely, ranging from minor changes in sensation to complete paralysis.
Early intervention and rehabilitation are really important for recovery and improving your quality of life. Prioritising health and wellness is key to managing the challenges that come with an SCI.