Mepolizumab
Sounds like 'ME-poe-LIZ-ue-mab'
Key points about mepolizumab
- Mepolizumab is used to treat a type of severe asthma called eosinophilic asthma.
- Keep taking your regular asthma medicines while you're using mepolizumab.
- Mepolizumab is also called Nucala.
- Find out how to take it safely and possible side effects.

Mepolizumab is used to treat a severe form of asthma called eosinophilic asthma. In this type of asthma, airway inflammation and breathing problems are triggered by high levels of white blood cells called eosinophils. In some people, too many eosinophils can cause asthma flare-ups. Eosinophilic asthma is rare and usually occurs in adults.
Mepolizumab helps by lowering the number of eosinophils that can cause asthma attacks. It works by targeting and blocking specific parts of the immune system which react when you have asthma. This can help reduce how often and how bad your asthma attacks are, improve your asthma symptoms and how you feel overall, and may reduce your need for steroid tablets such as prednisone.
Mepolizumab is available as an injection which is given under your skin every 4 weeks.
Mepolizumab does not give immediate relief from an asthma attack
- Don't use mepolizumab to treat sudden breathing problems.
- If you have an asthma action plan that you have agreed with your healthcare provider, follow it closely at all times.
- For severe asthma symptoms, you should use your reliever inhaler immediately and call an ambulance on 111 or go to your nearest Accident & Emergency clinic.
Keep taking your regular asthma medicines while you're using mepolizumab
- Take mepolizumab with your usual asthma medicines. Don't stop your usual medicines suddenly, as this can worsen your asthma.
- If your asthma gets better, your healthcare provider might slowly reduce some of your other medicines.
In Aotearoa New Zealand mepolizumab is funded under a Special Authority, for people who meet the criteria. A special authority means your specialist will need to make an application to Pharmac (the government medicine funding agency) for approval before the medicine can be funded for you. Read more about special authority.
Having the injection
- Mepolizumab comes as an injection pen which is pre-filled with the medicine.
- The injection is given under your skin (called subcutaneous) into your thigh or abdomen (tummy) every 4 weeks. If you have a caregiver giving you the injection it can also be given in your upper arm.
- On the day of your injection, take your asthma medication as usual. If you're taking steroid tablets, ask your healthcare provider if you need to decrease your dose.
- When you start mepolizumab, the first few injections will be given to you by your healthcare provider at the clinic. For some people, there is the rare risk of having an allergic reaction to mepolizumab. You’ll be monitored during the injection and asked to wait afterwards to make sure you don’t have any reaction.
- After a few months of treatment, if your response is good, you may be able to give yourself the injection at home, or it can be given by another person, for example, a whānau member or friend after proper training, or by your healthcare provider.
How to store mepolizumab
- Store mepolizumab in the fridge, in the original package. Don't freeze it. If your pen has been frozen, don't use it.
- Before injecting, take your mepolizumab pen out of the fridge and leave it at room temperature for 30 minutes. This helps reduce discomfort that can occur with a cold injection. Don't warm it in the microwave or in hot water.
- Mepolizumab may be stored out of the fridge for a maximum of 7 days. Write the date on the pack if you take it out of the fridge and use it within 7 days.
Injection sites
- Choose an injection site, such as on the front of your thighs or your abdomen (belly) at least 5 cm from your belly button. The injection site should be different from your last injection site, at least 5 cm away. Don't inject into skin that is sore, bruised, red, hard, scarred, has stretch marks, or psoriasis plaques.
Get rid of your used pen safely
- It's important to get rid of your used pen safely. Keep it out of reach of children and pets.
- It's best to put the used pen into a sharps container you can buy from your pharmacy. A sharps container is made of hard plastic that has a tight-fitting lid so used needles and pens can be stored safely. Don't put them in rubbish or recycle bins.
- Once your sharps container is full, take it to your pharmacy for safe disposal. Read more about safe disposal of pre-filled pens and other sharps.
Here are some things to know when you're taking mepolizumab. Other things may be important as well, so ask your healthcare provider what you should know about.
- Monitoring and review: Mepolizumab does not work immediately. It may take a few weeks before you notice any difference. Your healthcare provider will regularly check how well mepolizumab is working for you. If your symptoms don’t improve over time, the treatment may be stopped.
- Don’t stop your regular asthma medicines: Take mepolizumab with your usual asthma medicines. Don't stop your usual medicines suddenly, as this can worsen your asthma.
- Taking other medicines: Mepolizumab may interact with some medicines, herbal supplements and rongoā Māori, so check with your healthcare provider or pharmacist before starting mepolizumab and before starting any new products.
Like all medicines, mepolizumab can cause side effects, although not everyone gets them. If you're concerned about any symptoms, talk to your healthcare provider. The following information offers some guidance but doesn't include all possible side effects.
Common side effects
Tell your healthcare provider if any of these side effects bother you.
- Pain and discomfort at the injection site including redness, swelling, itching and a burning sensation of the skin near where the injection was given.
- Headache.
- Dizziness.
- Rash.
- Back pain.
- Sore throat.
- Cough.
- Stuffy nose.
Tell your healthcare provider immediately or phone Healthline free on 0800 611 116 if these occur
- Signs of an infection such as fever, cough, sore throat, diarrhoea (runny poo) or generally feeling weak and unwell.
Phone 111 for an ambulance or go to your nearest accident and emergency (A&E) clinic if these occur
- Signs of an allergic reaction such as difficulty breathing, rash, hives or itching.
For more information on side effects, see the Medsafe consumer information leaflet Nucala(external link).
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
The following links provide further information on Nucala.
Medsafe Consumer Information Sheets: Nucala(external link)
Brochures
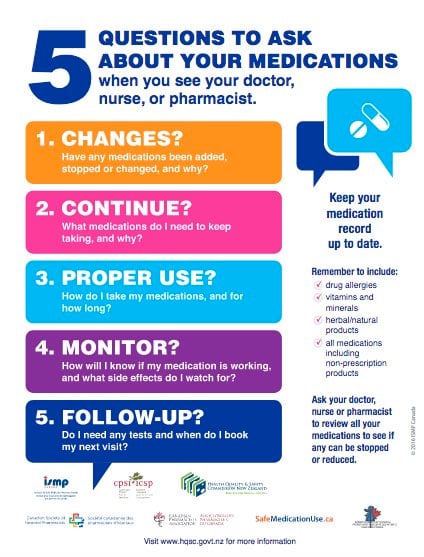
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
Medicines and side effects [PDF, 91 KB] Healthify He Puna Waiora, NZ, 2024
References
- Mepolizumab(external link) New Zealand Formulary
Brochures

Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed: