A continuous glucose monitor (CGM) is a small device people with diabetes can wear that measures their glucose levels every few minutes throughout the day and night. The readings are sent to a receiver which can be programmed to sound alarms and send alerts if your glucose levels are outside your set target range, eg, if they're getting too high or too low. The information can also be used to produce reports which show trends and patterns in your glucose levels to help you get better diabetes control. Read more about how a CGM works.
What are the benefits of CGMs?
The aim of diabetes management is to keep your glucose levels in a healthy range. To do this well you need to monitor your glucose levels regularly. You can do this with finger-prick tests and a blood glucose monitor. This gives you a snapshot of your glucose levels at the time of the test. Because CGMs continuously track your glucose levels, including telling you whether the level is rising or falling, people who use a CGM often have better blood glucose management compared to using finger-prick testing.
- You can see trends and patterns in your glucose levels for better diabetes management: The information collected from the CGM will show you what your glucose level is right now and will put all your readings together into a graph. This lets you see how much time each day your blood glucose level stays within range, and records times when it goes too high or too low. This shows a full picture of how your glucose levels change over time and how food and drink, physical activity, stress, and being sick change your results.
- You can notice and respond to changing glucose levels quickly: Most CGMs can send you or your caregiver an alert when your glucose levels get too high or low. This makes it much easier to act before there is a problem.
Finger prick tests are still important
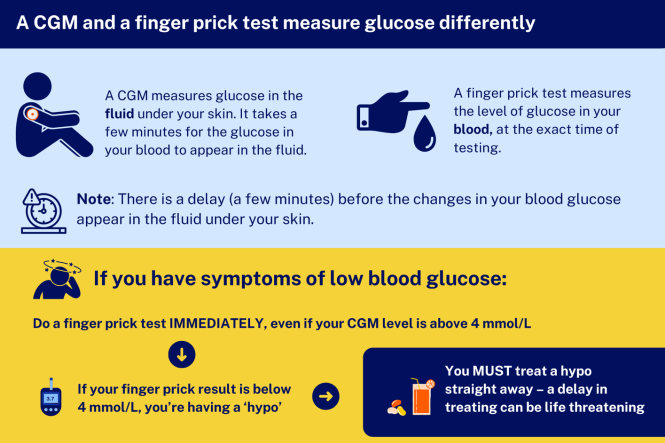
Image credit: Healthify He Puna Waiora
For more information, see the section below, can I stop doing finger prick checks to monitor my blood glucose if I have a CGM?
Funding of CGMs for people in New Zealand
- Find out who can get funded CGMs below.
- CGMs can be used by themselves (called standalone CGMs) or may be used with a compatible insulin pump.
- CGMs are currently not funded for people with type 2 diabetes. Read more about why type 2 diabetes isn't included(external link).
You can also read about diabetes technology(external link) and glucose monitoring for children with diabetes(external link) on the KidsHealth New Zealand site.